Chemical Pregnancy After IVF And IUI: Is It A Good Sign?
Read about the complete information related to Chemical Pregnancy After IVF And IUI. What is IVF and other imporant information.
Pregnancy is a happy moment. But, the path to pregnancy isn’t always easy. For many couples, pregnancy is a distant dream. Unfortunately, infertility deprives many families of the spontaneous pleasure of creating new life and adding to the merry brood.
Unlike most couples yearning for a baby, couples who have infertility have to walk that extra mile to fulfil their dreams of having a family. And, one of the methods that can help overcome infertility is an IVF or In Vitro Fertilization treatment.
But IVF is not the holy-grail, it is not a fool-proof method. Many IVF treatments do end in heartbreak. One of the biggest challenges of IVF treatment is a chemical pregnancy. If you are thinking of opting for an IVF or have already chosen the option, you need to know more about this unusual heart-breaking phenomenon called ‘Chemical Pregnancy.’ So here, we have provided some important information on the subject. Read on to learn more.
What Is IVF?
Before we know about chemical pregnancy, let’s understand IVF a little better.
IVF or In Vitro Fertilization is a proof that medical science can do wonder. The process includes hormone therapy which encourages the development of numerous eggs in a woman’s ovaries.
These eggs are then collected and fertilized in a test tube using healthy sperms received from a man. These fecundated eggs go on to make embryos that are permitted to grow for 2-5 days. The most vigorous of these embryos are transferred to the uterus. Pregnancy typically starts when these embryos nestle in nicely in the uterus (implantation).
A Chemical Pregnancy:-
Now that you know, what IVF is, let’s know about a chemical pregnancy. What exactly is a chemical pregnancy? How is it different from a miscarriage?
A chemical pregnancy is a practical name given to a heart-breaking condition– a pregnancy loss. Here’s a brief account of what a chemical pregnancy necessitates:
- A chemical pregnancy is an early miscarriage, a rather early miscarriage. In fact, more women than you can suppose, have a chemical pregnancy but, don’t even have knowledge about it.
- It usually happens around the time of your periods and sometimes little after it. That is when you are technically five to six weeks pregnant.
- A chemical pregnancy signalizes that your body did make the hCG hormone, a sure shot indicator of pregnancy.
- Most women experience their periods within days of a positive pregnancy test when they have a chemical pregnancy.
A chemical pregnancy does not have differentiating symptoms. It feels like a period that came a little late.
Women who are facing
infertility, especially those undergoing IVF, realize a chemical pregnancy more often than others. Women who conceive naturally, in most cases, treat a chemical pregnancy as a late period because they have no clue they were even pregnant in the first place! On the other hand, women using artificial reproductive techniques like IUI and IVF, test (whether HPT or a blood test) a maximum of 14 days after transfer, which allows them to realise an early pregnancy.
Chemical Pregnancy and IVF – Causes
Many women experience chemical pregnancy while undergoing IVF. Around 20 out of 100 IVF treatment couples experience a positive pregnancy test post transfer, end up with an early pregnancy loss or chemical pregnancy.
Here are the main reasons of a chemical pregnancy after IVF:
1. Embryo Abnormalities:
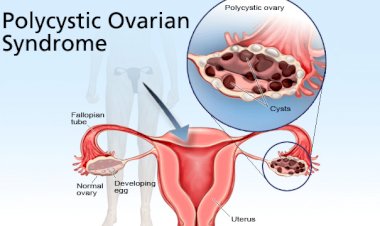
The biggest reason of a chemical pregnancy and miscarriage is embryo abnormality. What exactly does embryo abnormality mean? Well, a normal embryo consists of many chromosomes. But an abnormal embryo contains a disproportionate number of chromosomes. Other factors that can affect the growth of abnormal embryos are structural chromosomal, epigenetic, and metabolic factors. Older women and women with PCOS (polycystic ovarian syndrome) are more likely to experience embryo abnormalities during IVF too.
2. Implantation Dysfunction:
Many chemical pregnancies occur due to implantation issues. Some of the causes of implantation dysfunction include:
- Endometrial polyps
- Fibroids
- Surgical scarring
- Advanced maternal age
- PCOS
3. Autoimmune Issues:
Sometimes, a woman’s immune cells are wired in such a way that they attack a growing embryo instead of nurturing it. This occurs because the immune system fails to differentiate between embryo cells and disease-causing cells.
4. Other Issues:
Other causes of chemical pregnancy include:
- Infections (especially sexually transmitted infections)
- Thyroid issues
- Abnormal hormone levels
- Luteal phase defects
- Unbalanced embryo chromosomal translocations
Testing to Avoid a Chemical Pregnancy
If you are experiencing repeated chemical pregnancies, it is time to to understand the phenomenon a little deeper.
Some tests that can help in detection of the real cause of repeated chemical pregnancies are:
1. Sonohysterogram, Hysteroscopy or APelvic MRI:
Any of these tests can help evaluate the condition of your uterus and identity any sort of unusualness. It is sensible to undergo these tests before you embark on IVF so that you can avoid chemical pregnancies and early pregnancy losses.
2. Ultrasound Scan:
An ultrasound scan determines the thickness of your endometrial wall lining. If your lining measures are less than 8mm, it makes sense to wait till it gets thicker before embryo transfer. A great method to thicken the lining is to use vaginal viagra 72 hours before the hCG trigger.
3. Natural Killer Cell Activity Test:
This primary immune test can help your doctor to find out if it is your immune system that is causing the chemical pregnancies.
4. Blood Tests:
If you are going through IVF, the chances are higher that you would have already undergone a plethora of blood tests. But it is likely that something has changed in your body since your last series of tests. So, it is better to go through fresh tests to detect more about your repeated chemical pregnancies.
5. Molecular and Biochemical Testing:
The doctor can also investigate the molecular and biochemical factors in your endometrium. These tests can help in determining your chances of implantations.
6. Chromosome Testing:
Thanks to the development of medical science that your doctor can now choose the healthiest embryo to transfer. Tests like using Comparative Genomic Hybridization (CGH) can help identify chromosomally healthy and normal embryos.
IVF and Chemical Pregnancy – Prevention
Once the exact cause is identified, your doctor can go on to treat the condition. Some of the treatment options for recurring chemical pregnancies are:
1. Progesterone:
If your body is not originating enough progesterone and that is causing your early pregnancy losses, your doctor may recommend oral or vaginal progesterone use.
2. Baby Aspirin:
Baby Aspirin works as a blood thinner and can help stop chemical pregnancy.
3. Antibiotics:
If an infection is causing you to lose your pregnancies, a course of antibiotics can do the trick.
4. Surgery:
In many cases, abnormalities in the uterus can cause chemical pregnancies. In such a case, your doctor may prescribe surgery to determine the problem.
Women who have never gone through the heartbreak that is a chemical pregnancy often surprise what the fuss is all about. You weren’t really that far along so you should not grieve – is, unfortunately, the common mindset about chemical pregnancy. But what you lost was also your baby.You are allowed to mourn the loss of life that never got a fair chance at life.
But keep in mind, this is not the end. Most women who face a chemical pregnancy go on to have healthy babies. So never give up. Consult your doctor, and get ready for the next round.
Your suggestions and experiences are valuable to us. Please do share with us in the comment box.


































Comments (0)